AI-Powered Diagnostics in Pediatric Healthcare
A case study
Case Study: AI-Powered Diagnostics in Pediatric Healthcare
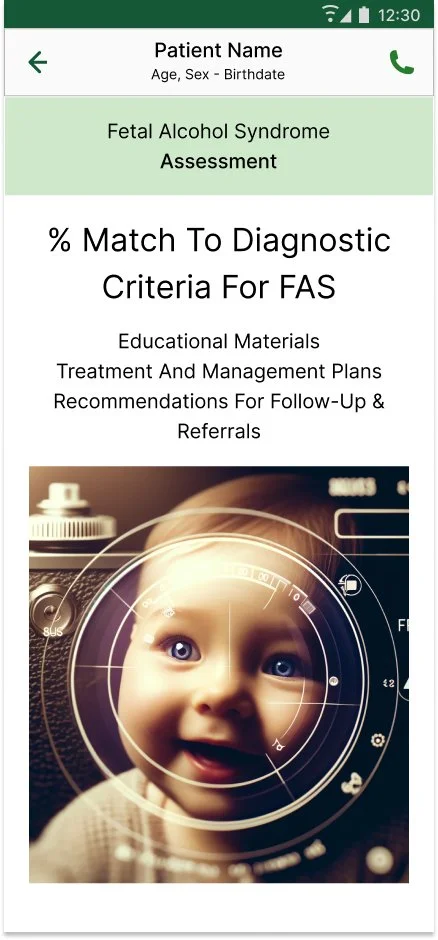
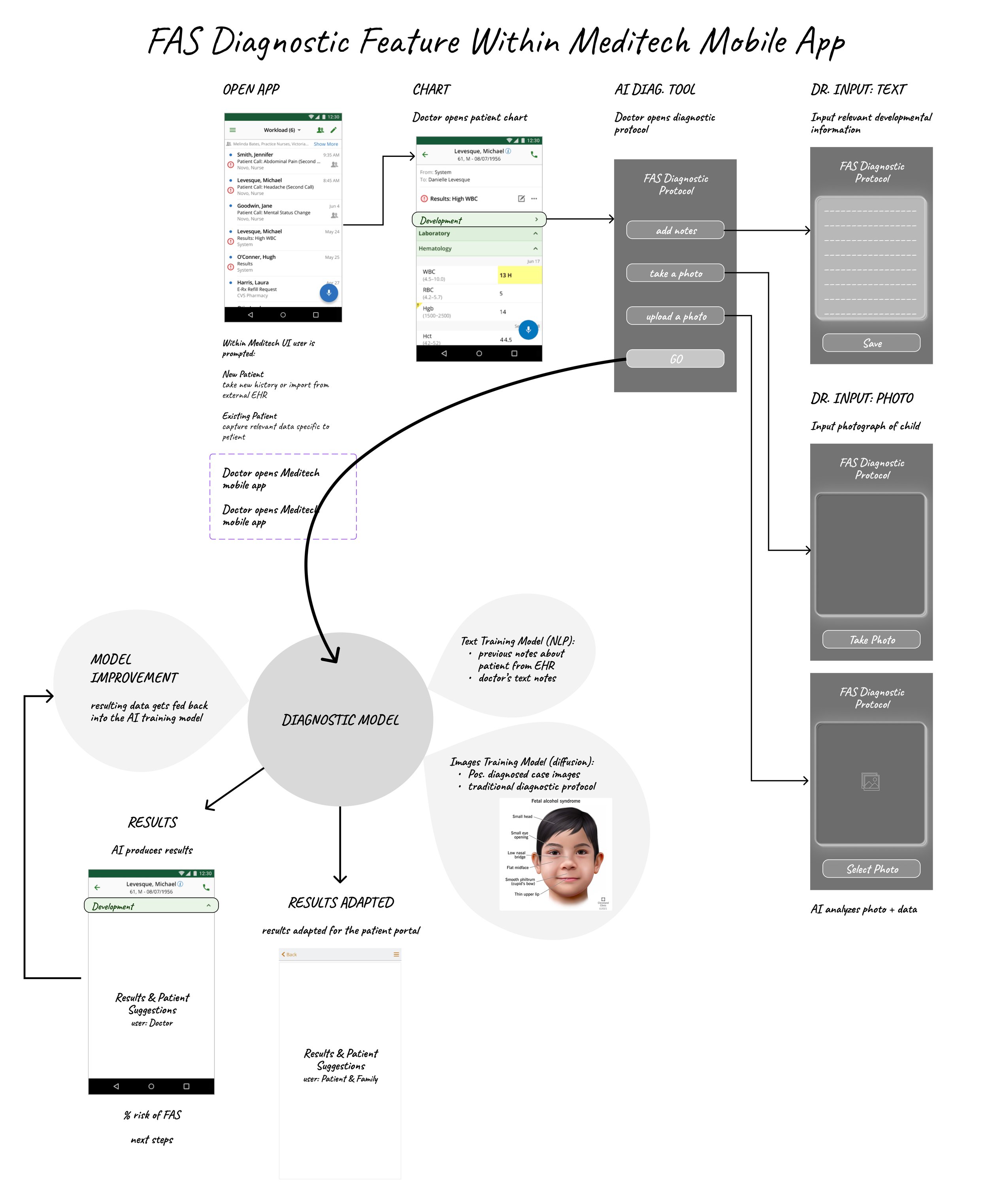
In this case study, I explore the theoretical application of artificial intelligence (AI) technologies in pediatric healthcare, focusing on the potential to enhance the diagnosis of Fetal Alcohol Syndrome (FAS). This study serves as a conceptual exploration into how integrating AI, specifically through Natural Language Processing (NLP) and image recognition, could improve diagnostic accuracy and efficiency within the Meditech Mobile App environment.
The purpose of this project was to investigate how multimodal AI systems could aid in the complex and nuanced field of pediatric diagnosis by providing a tool that analyzes both textual and visual data. This approach aimed to reduce diagnostic errors and provide a faster, more reliable assessment process, enabling healthcare providers to make better-informed decisions with greater confidence.
By detailing the development, potential implementation, and theoretical outcomes of this AI tool, as well as addressing the ethical and data privacy concerns associated with AI in healthcare, this case study not only highlights my capabilities in conceptualizing and designing AI applications but also underscores my commitment to innovating healthcare solutions that prioritize patient care and data integrity.
This case study exemplifies my interdisciplinary expertise in AI, software development, and healthcare, showcasing my dedication to pushing the boundaries of technology to solve real-world problems.
Persona Overview
Name: Dr. Elena Martinez
Age: 38
Role: Pediatrician
Location: Urban medical center with a diverse patient population
Professional Background
Experience: 10+ years in pediatrics, with specialized training in developmental disorders.
Special Interest: Early diagnosis and intervention for children with developmental and behavioral issues.
Technology Proficiency: Comfortable using advanced medical technologies and EHR systems. Always looking for tools to enhance patient care and streamline administrative tasks.
Goals
Primary Goal: To accurately diagnose and manage conditions as early as possible to optimize patient outcomes.
Secondary Goal: To efficiently document and track patient progress over time, using data to inform treatment plans.
Needs
Informational Needs: Access to the latest guidelines and diagnostic criteria for Fetal Alcohol Syndrome within the EHR. Need for integrative tools that can analyze patient history, symptoms, and diagnostic tests to aid in diagnosis.
Functional Needs: A user-friendly interface that allows for easy input of patient symptoms and outputs potential diagnoses. The tool should integrate with the rest of the EHR system for seamless access to patient history and documentation.
Emotional Needs: Assurance that the tool is reliable and evidence-based, giving confidence in diagnoses made. Support for dealing with the complexities and sensitivities involved in diagnosing and discussing Fetal Alcohol Syndrome with families.
Pain Points
Complexity of Diagnosis: FAS can be difficult to diagnose due to the variability in symptoms and the need for comprehensive evaluation.
Time Constraints: Limited time for each patient visit, making it challenging to conduct thorough assessments for conditions like FAS.
Documentation: The need for detailed documentation for both clinical management and billing purposes, which can be time-consuming.
Scenario
Dr. Martinez encounters a 6-month-old patient with several developmental delays and physical abnormalities suggestive of Fetal Alcohol Syndrome. She needs to quickly review the child's history, conduct an assessment, and utilize diagnostic tools within the EHR to consider a diagnosis of FAS. She values a tool that can guide her through the diagnostic criteria, suggest additional tests or evaluations, and help explain the potential diagnosis to the child's caregivers.
In the Exam Room:
Dr. Martinez
6-Month-Old Patient
Parent
Diagnostic Protocols
The Centers for Disease Control and Prevention (CDC) refers to the guidelines established by the National Task Force on Fetal Alcohol Syndrome and Fetal Alcohol Effect and the Institute of Medicine (IOM) for diagnosing Fetal Alcohol Syndrome (FAS). These guidelines focus on specific features and criteria that need to be present for a diagnosis of FAS.
The criteria include:
Evidence of Prenatal Alcohol Exposure
Confirmed maternal alcohol exposure during pregnancy is ideal but not always necessary for a diagnosis if other key features are present. This also presents a challenge, as a Doctor will need to communicate this concern to a mother without accusing her of prenatal abuse.Facial Anomalies
Three distinct facial anomalies are characteristic of FASShort palpebral fissures: Smaller than average openings of the eyes
Smooth philtrum: The vertical groove between the base of the nose and the border of the upper lip is flattened or smooth
Thin upper lip: The upper lip is thinner than average and less pronounced.
Growth Deficiencies
Growth deficiencies are often present, either prenatal (e.g., low birth weight) or postnatal (e.g., failure to thrive), with the child being below the 10th percentile for height, weight, or both, adjusted for age and genetic background.Central Nervous System (CNS) Abnormalities
The CNS abnormalities can be structural, neurological, or functional, including:Structural CNS abnormalities: Documented brain abnormalities (e.g., reduction in brain size, abnormal structure)
Neurological problems: Neurological issues that are not attributable to a postnatal insult or fever, or other soft neurological signs, such as impaired fine motor skills
Functional CNS abnormalities: Evidence of a complex pattern of behavioral or cognitive abnormalities that are inconsistent with developmental level and cannot be explained by family background or environment alone. These might include severe deficits in:
Learning disabilities
Memory
Impulse control
Social perception
Communication skills
Problem-solving skills
Attention and hyperactivity
Exclusion of Alternative Diagnoses
The diagnosis requires that these signs and symptoms cannot be better explained by another condition. This is important to differentiate FAS from other developmental disorders that might present with similar symptoms.
AI Model Documentation
Text Training Model (NLP):
previous notes about FAS patients from EHR
text diagnostic materials for FAS
Images Training Model (diffusion):
Positive diagnosed case images
traditional diagnostic protocol
Data Preprocessing
Data Normalization and Standardization: Input data (e.g., patient history, physical examination findings, developmental assessments) are normalized to ensure consistency across different sources and formats.
Feature Extraction: Relevant features are extracted from the input data. For structured data, this might be straightforward. For unstructured data, such as doctor's notes, NLP techniques like entity recognition are used to identify and extract pertinent information.
Models and Techniques
Natural Language Processing (NLP)
Use: To interpret unstructured data such as clinical notes, extracting relevant information about symptoms, patient history, and other diagnostic criteria.
Techniques: Techniques might include named entity recognition (NER) to identify medical terms, sentiment analysis to gauge the severity of symptoms described, and text classification to categorize notes into relevant diagnostic categories.Machine Learning Models for Pattern Recognition
Use: To identify patterns in the data that correlate with diagnoses of FAS.Models:
Supervised Learning Models, like decision trees, random forests, or gradient boosting machines can classify cases as FAS or not FAS based on labeled training data.
Deep Learning Models, particularly convolutional neural networks (CNNs), could be used for analyzing imaging data (if applicable) to identify physical markers of FAS.
Clinical Decision Support Algorithms
Use: To integrate the outputs of various models, along with clinical guidelines and diagnostic criteria, into actionable recommendations.Implementation: These algorithms might use rule-based systems informed by current medical standards for diagnosing FAS. They could also incorporate a probabilistic approach to account for uncertainty and variance in symptoms presentation.
Cohort Data & Patient Data
Patient Demographics
Age: Infants, children, and potentially adolescents, given the range of presentation times for FAS symptoms
Gender: Both male and female patients, as FAS affects individuals regardless of gender
Ethnicity: Diverse ethnic backgrounds to ensure the model can accurately interpret symptoms across different populations.
Maternal History
Alcohol Use: Documented history of alcohol consumption during pregnancy, including frequency and quantity, if available.
Pregnancy and Birth Records: Other relevant maternal factors, including drug use, prenatal care records, and any complications during pregnancy or birth.
Medical History
Developmental Milestones: Records indicating any delays or abnormalities in reaching developmental milestones
Medical Conditions: Existing medical conditions, especially those related to or could be confused with FAS, to teach the model differential diagnosis.
Physical Examination Findings
Growth Metrics: Height, weight, and head circumference, specifically looking for growth retardation
Facial Features: Specific facial anomalies associated with FAS, such as smooth philtrum, thin upper lip, and small palpebral fissures.
Neurological and Structural Abnormalities: Any documented neurological issues or physical deformities.
Diagnostic Test
Imaging: Brain imaging studies (e.g., MRI, CT scans) that could indicate abnormalities
Genetic Testing: Data from genetic tests, if conducted, to rule out other syndromes.
Developmental and Behavioral Assessments
Cognitive Assessments: IQ tests and other assessments of cognitive function
Behavioral Evaluations: Reports on behavior, including any issues with attention, hyperactivity, or social interactions.
Treatment and Intervention History
Therapies: Details on any interventions, such as speech therapy, occupational therapy, or special education services
Outcomes: Follow-up data on the effectiveness of interventions.
Integration with EHR
APIs and Interoperability: The AI system must be tightly integrated with the EHR through APIs that allow for the seamless exchange of data. Standards like FHIR (Fast Healthcare Interoperability Resources) can facilitate this exchange.
Feedback Loops: The system could include mechanisms for clinicians to provide feedback on its suggestions, which can be used for continuous learning and improvement of the models.
Data Privacy & Ethical Considerations
Collecting and using this data requires stringent adherence to privacy laws and ethical standards, including anonymization of patient data and securing consent where necessary. The cohort should be large and diverse enough to enable the model to learn the complex patterns associated with FAS, including subtle variations in symptom presentation across different demographics.
Continuous Learning and Adaptation
Model Retraining: Regularly updating the machine learning models with new data to improve accuracy and adapt to changing clinical guidelines.
Performance Monitoring: Continuous monitoring of the AI system’s performance, including accuracy, usability, and clinical outcomes, to ensure it meets the required standards and supports clinical needs effectively.
Conclusion
This case study underscores the transformative potential of artificial intelligence in enhancing pediatric healthcare diagnostics. By theoretically integrating NLP and image recognition technologies into the Meditech Mobile App, the proposed AI tool aimed to revolutionize the diagnostic process for Fetal Alcohol Syndrome (FAS), making it both more efficient and accurate.
The exploration of this AI integration highlights not only the feasibility of such technologies in medical settings but also the critical importance of ethical considerations and continuous learning. As we continue to navigate the complexities of AI in healthcare, this case study serves as a testament to the necessity of balancing innovation with careful consideration of privacy, data security, and the overall well-being of patients.
As a professional dedicated to leveraging technology to improve healthcare, this project exemplifies my commitment to creating solutions that are not only technologically advanced but also socially responsible and patient-centric. It reinforces my belief that the future of healthcare lies in the seamless integration of technology and patient care, driven by AI’s potential to provide deeper insights and more accurate diagnoses.
Moving forward, I am eager to take the insights gained from this theoretical exploration and apply them to real-world applications, continuing to contribute to the evolution of healthcare technology.